よむ、つかう、まなぶ。
【参考資料3】【英版R4.1.17】Nippon AMR One Health Report (NAOR) 2020 (80 ページ)
出典
| 公開元URL | https://www.mhlw.go.jp/stf/newpage_23261.html |
| 出典情報 | 国際的に脅威となる感染症対策関係閣僚会議 薬剤耐性ワンヘルス動向調査検討会(第9回 1/17)《厚生労働省》 |
ページ画像
ダウンロードした画像を利用する際は「出典情報」を明記してください。
低解像度画像をダウンロード
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
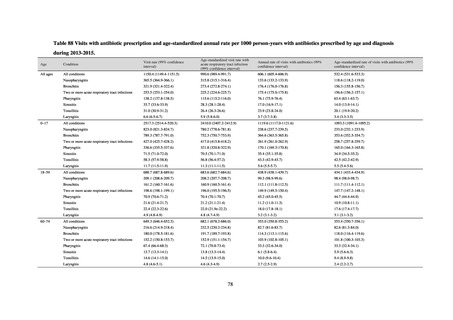
[Summary]
Although the antimicrobial usage rate for acute respiratory tract infections differs slightly between studies, these
differences are thought to be due to differences in the timing of the studies’ implementation and in their definitions of
respiratory tract infection. However, as all these studies show usage diminishing over time, the situation in respect of the
unnecessary use of antimicrobials for respiratory tract infections is believed to be improving. Nevertheless, given that
almost all acute respiratory tract infections are viral infections, further reductions would appear to be possible, so similar
studies will continue to be needed. The high prescription rate among patients aged between 13 and 39 could become a
target for future efforts to support stewardship.
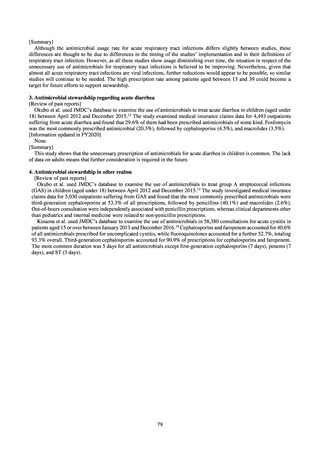
3. Antimicrobial stewardship regarding acute diarrhea
[Review of past reports]
Okubo et al. used JMDC’s database to examine the use of antimicrobials to treat acute diarrhea in children (aged under
18) between April 2012 and December 2015. 12 The study examined medical insurance claims data for 4,493 outpatients
suffering from acute diarrhea and found that 29.6% of them had been prescribed antimicrobials of some kind. Fosfomycin
was the most commonly prescribed antimicrobial (20.3%), followed by cephalosporins (4.5%), and macrolides (3.5%).
[Information updated in FY2020]
None
[Summary]
This study shows that the unnecessary prescription of antimicrobials for acute diarrhea in children is common. The lack
of data on adults means that further consideration is required in the future.
4. Antimicrobial stewardship in other realms
[Review of past reports]
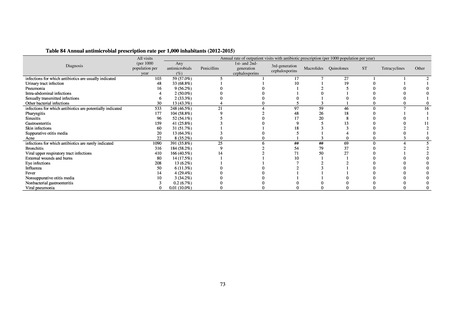
Okubo et al. used JMDC’s database to examine the use of antimicrobials to treat group A streptococcal infections
(GAS) in children (aged under 18) between April 2012 and December 2015.13 The study investigated medical insurance
claims data for 5,030 outpatients suffering from GAS and found that the most commonly prescribed antimicrobials were
third-generation cephalosporins at 53.3% of all prescriptions, followed by penicillins (40.1%) and macrolides (2.6%).
Out-of-hours consultation were independently associated with penicillin prescriptions, whereas clinical departments other
than pediatrics and internal medicine were related to non-penicillin prescriptions.
Kusama et al. used JMDC’s database to examine the use of antimicrobials in 58,380 consultations for acute cystitis in
patients aged 15 or over between January 2013 and December 2016.14 Cephalosporins and faropenem accounted for 40.6%
of all antimicrobials prescribed for uncomplicated cystitis, while fluoroquinolones accounted for a further 52.7%, totaling
93.3% overall. Third-generation cephalosporins accounted for 90.9% of prescriptions for cephalosporins and faropenem.
The most common duration was 5 days for all antimicrobials except first-generation cephalosporins (7 days), penems (7
days), and ST (3 days).
79
Although the antimicrobial usage rate for acute respiratory tract infections differs slightly between studies, these
differences are thought to be due to differences in the timing of the studies’ implementation and in their definitions of
respiratory tract infection. However, as all these studies show usage diminishing over time, the situation in respect of the
unnecessary use of antimicrobials for respiratory tract infections is believed to be improving. Nevertheless, given that
almost all acute respiratory tract infections are viral infections, further reductions would appear to be possible, so similar
studies will continue to be needed. The high prescription rate among patients aged between 13 and 39 could become a
target for future efforts to support stewardship.
3. Antimicrobial stewardship regarding acute diarrhea
[Review of past reports]
Okubo et al. used JMDC’s database to examine the use of antimicrobials to treat acute diarrhea in children (aged under
18) between April 2012 and December 2015. 12 The study examined medical insurance claims data for 4,493 outpatients
suffering from acute diarrhea and found that 29.6% of them had been prescribed antimicrobials of some kind. Fosfomycin
was the most commonly prescribed antimicrobial (20.3%), followed by cephalosporins (4.5%), and macrolides (3.5%).
[Information updated in FY2020]
None
[Summary]
This study shows that the unnecessary prescription of antimicrobials for acute diarrhea in children is common. The lack
of data on adults means that further consideration is required in the future.
4. Antimicrobial stewardship in other realms
[Review of past reports]
Okubo et al. used JMDC’s database to examine the use of antimicrobials to treat group A streptococcal infections
(GAS) in children (aged under 18) between April 2012 and December 2015.13 The study investigated medical insurance
claims data for 5,030 outpatients suffering from GAS and found that the most commonly prescribed antimicrobials were
third-generation cephalosporins at 53.3% of all prescriptions, followed by penicillins (40.1%) and macrolides (2.6%).
Out-of-hours consultation were independently associated with penicillin prescriptions, whereas clinical departments other
than pediatrics and internal medicine were related to non-penicillin prescriptions.
Kusama et al. used JMDC’s database to examine the use of antimicrobials in 58,380 consultations for acute cystitis in
patients aged 15 or over between January 2013 and December 2016.14 Cephalosporins and faropenem accounted for 40.6%
of all antimicrobials prescribed for uncomplicated cystitis, while fluoroquinolones accounted for a further 52.7%, totaling
93.3% overall. Third-generation cephalosporins accounted for 90.9% of prescriptions for cephalosporins and faropenem.
The most common duration was 5 days for all antimicrobials except first-generation cephalosporins (7 days), penems (7
days), and ST (3 days).
79