よむ、つかう、まなぶ。
【参考資料3】【英版R4.1.17】Nippon AMR One Health Report (NAOR) 2020 (28 ページ)
出典
| 公開元URL | https://www.mhlw.go.jp/stf/newpage_23261.html |
| 出典情報 | 国際的に脅威となる感染症対策関係閣僚会議 薬剤耐性ワンヘルス動向調査検討会(第9回 1/17)《厚生労働省》 |
ページ画像
ダウンロードした画像を利用する際は「出典情報」を明記してください。
低解像度画像をダウンロード
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
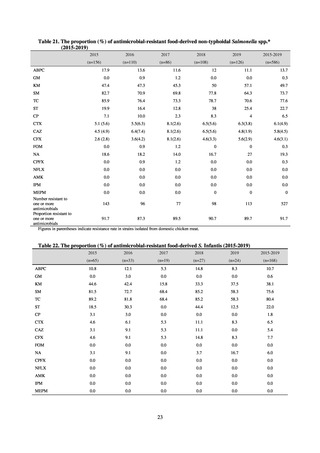
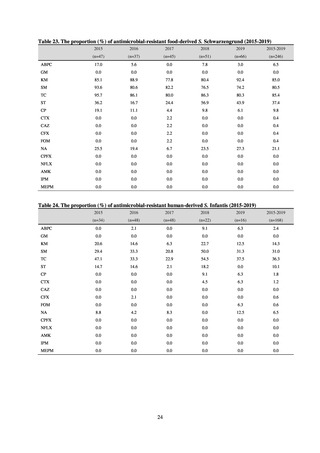
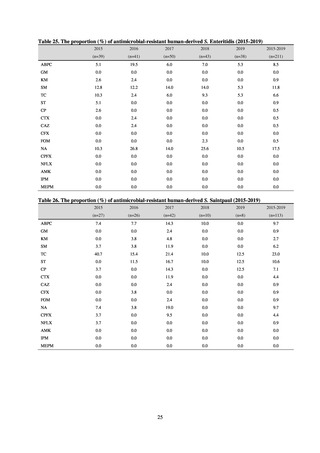
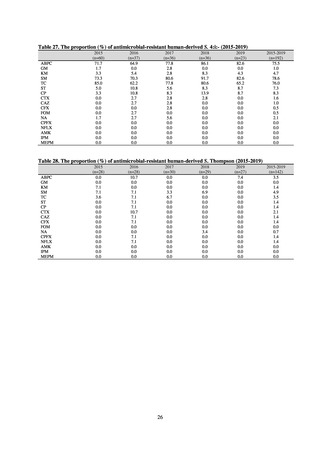
Table 29. Resistance rates among S. Infantis, S. Schwarzengrund, and S. Manhattan detected in humans
and food (2015-2019) (%)
Infantis
Human (n=168)
Food (n=168)
2.4
10.7
0.0
0.6
14.3
38.1
31.0
75.6
36.3
80.4
10.1
22.0
1.8
1.8
1.2
6.5
0.0
5.4
0.6
7.7
0.6
0.0
6.5
6.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
ABPC
GM
KM
SM
TC
ST
CP
CTX
CAZ
CFX
FOM
NA
CPFX
NFLX
AMK
IPM
MEPM
Schwarzengrund
Human (n=82)
Food (n=246)
3.7
6.5
0.0
0.0
61.0
85.0
70.7
80.5
69.5
85.4
26.8
37.4
1.2
9.8
2.4
0.4
2.4
0.4
0.0
0.4
0.0
0.4
14.6
21.1
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
Manhattan
Human (n=41)
Food (n=57)
2.4
10.5
0.0
0.0
0.0
0.0
87.8
93.0
82.9
77.2
0.0
1.8
0.0
0.0
0.0
10.5
0.0
10.5
0.0
0.0
0.0
0.0
9.8
12.3
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
ⅲ. Neisseria gonorrhoeae
Source: National Institute of Infectious Diseases
The 618, 675, 982, 1,167, and 1,023 Neisseria gonorrhoeae strains that were respectively isolated in 2015, 2016,
2017, 2018, and 2019 were tested for antimicrobial susceptibility (based on EUCAST breakpoints; Table 30).
Ceftriaxone (CTRX)-resistant strains respectively accounted for 6.2%, 4.3%, 4.3%, 3.5%, and 5.4%. Strains
assessed as resistant based on the CLSI Criteria (MIC ≥ 0.5 μg/mL) accounted for 0.6%, 0.4%, 0.5%, 0.3%, and
0.4%. No spectinomycin (SPCM)-resistant strains were present. On the other hand, the proportion (%) of
azithromycin (AZM)-resistant strains increased from 13.0% in 2015 to between 33% and 43.9% since 2016.
The CLSI Criteria do not provide a resistance breakpoint for azithromycin (AZM), but, using the azithromycin
(AZM) MIC distribution of strains with the 23S rRNA gene mutation as the basis, strains with a MIC of 2 μg/mL
or higher are referred to as “non-wild-type.” When we investigated the resistance rate (see Reference (8)), albeit
as a reference, we found that, between 2015 and 2019, 3.2%, 4.0%, 4.0%, 6.3%, and 7.5% of strains, respectively,
had a MIC of 2 μg/mL or higher, indicating an upward trend. According to clinical assessments in Japan, strains
indicating an azithromycin (AZM) MIC of 1 μg/mL or higher can reasonably be regarded as resistant. Under this
criterion (R ≥ 1 μg/mL), azithromycin-resistant strains accounted for 11.0%, 9.3%, 11.2%, 15.9%, and 14.9% of
strains respectively between 2015 and 2019. Among the other three antimicrobials, the proportion of CFIXresistant strains accounted for approximately 30-40%, and that of CPFX-resistant strains accounted for
approximately 60-80%. Penicillins (PCG) would not have a therapeutic effect on more than 80% of strains.
Table 30. The proportion (%) of antimicrobial-resistant Neisseria gonorrhoeae
CTRX
2015
(618 strains)
6.2
2016
(675 strains)
4.3
2017
(982 strains)
4.3
2018
(1,167 strains)
3.5
2019
(1,023 strains)
5.4
SPCM
0.0
0.0
0.0
0.0
0.0
AZM
13.0
33.5
42.6
43.9
40.1
PCG*
38.4 (96.6)
36.3 (96.9)
37.8(99.0)
31.7(82.5)
35.8(88.5)
CFIX
36.2
43.2
31.0
28.4
33.4
CPFX
79.5
78.0
75.8
66.9
64.6
The EUCAST (Appendix 8) standards were used for susceptibility and resistance assessment.
* Figures in parentheses indicate the sum of resistance and intermediate resistance.
The EUCAST resistance breakpoints are as follows. CTRX (>0.125 μg/mL), SPCM (> 64 μg/mL), AZM (>0.5 μg/mL), PCG (> 1 μg/mL),
CFIX (>0.125 μg/mL), CPFX (> 0.06 μg/mL)
27
and food (2015-2019) (%)
Infantis
Human (n=168)
Food (n=168)
2.4
10.7
0.0
0.6
14.3
38.1
31.0
75.6
36.3
80.4
10.1
22.0
1.8
1.8
1.2
6.5
0.0
5.4
0.6
7.7
0.6
0.0
6.5
6.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
ABPC
GM
KM
SM
TC
ST
CP
CTX
CAZ
CFX
FOM
NA
CPFX
NFLX
AMK
IPM
MEPM
Schwarzengrund
Human (n=82)
Food (n=246)
3.7
6.5
0.0
0.0
61.0
85.0
70.7
80.5
69.5
85.4
26.8
37.4
1.2
9.8
2.4
0.4
2.4
0.4
0.0
0.4
0.0
0.4
14.6
21.1
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
Manhattan
Human (n=41)
Food (n=57)
2.4
10.5
0.0
0.0
0.0
0.0
87.8
93.0
82.9
77.2
0.0
1.8
0.0
0.0
0.0
10.5
0.0
10.5
0.0
0.0
0.0
0.0
9.8
12.3
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
ⅲ. Neisseria gonorrhoeae
Source: National Institute of Infectious Diseases
The 618, 675, 982, 1,167, and 1,023 Neisseria gonorrhoeae strains that were respectively isolated in 2015, 2016,
2017, 2018, and 2019 were tested for antimicrobial susceptibility (based on EUCAST breakpoints; Table 30).
Ceftriaxone (CTRX)-resistant strains respectively accounted for 6.2%, 4.3%, 4.3%, 3.5%, and 5.4%. Strains
assessed as resistant based on the CLSI Criteria (MIC ≥ 0.5 μg/mL) accounted for 0.6%, 0.4%, 0.5%, 0.3%, and
0.4%. No spectinomycin (SPCM)-resistant strains were present. On the other hand, the proportion (%) of
azithromycin (AZM)-resistant strains increased from 13.0% in 2015 to between 33% and 43.9% since 2016.
The CLSI Criteria do not provide a resistance breakpoint for azithromycin (AZM), but, using the azithromycin
(AZM) MIC distribution of strains with the 23S rRNA gene mutation as the basis, strains with a MIC of 2 μg/mL
or higher are referred to as “non-wild-type.” When we investigated the resistance rate (see Reference (8)), albeit
as a reference, we found that, between 2015 and 2019, 3.2%, 4.0%, 4.0%, 6.3%, and 7.5% of strains, respectively,
had a MIC of 2 μg/mL or higher, indicating an upward trend. According to clinical assessments in Japan, strains
indicating an azithromycin (AZM) MIC of 1 μg/mL or higher can reasonably be regarded as resistant. Under this
criterion (R ≥ 1 μg/mL), azithromycin-resistant strains accounted for 11.0%, 9.3%, 11.2%, 15.9%, and 14.9% of
strains respectively between 2015 and 2019. Among the other three antimicrobials, the proportion of CFIXresistant strains accounted for approximately 30-40%, and that of CPFX-resistant strains accounted for
approximately 60-80%. Penicillins (PCG) would not have a therapeutic effect on more than 80% of strains.
Table 30. The proportion (%) of antimicrobial-resistant Neisseria gonorrhoeae
CTRX
2015
(618 strains)
6.2
2016
(675 strains)
4.3
2017
(982 strains)
4.3
2018
(1,167 strains)
3.5
2019
(1,023 strains)
5.4
SPCM
0.0
0.0
0.0
0.0
0.0
AZM
13.0
33.5
42.6
43.9
40.1
PCG*
38.4 (96.6)
36.3 (96.9)
37.8(99.0)
31.7(82.5)
35.8(88.5)
CFIX
36.2
43.2
31.0
28.4
33.4
CPFX
79.5
78.0
75.8
66.9
64.6
The EUCAST (Appendix 8) standards were used for susceptibility and resistance assessment.
* Figures in parentheses indicate the sum of resistance and intermediate resistance.
The EUCAST resistance breakpoints are as follows. CTRX (>0.125 μg/mL), SPCM (> 64 μg/mL), AZM (>0.5 μg/mL), PCG (> 1 μg/mL),
CFIX (>0.125 μg/mL), CPFX (> 0.06 μg/mL)
27