よむ、つかう、まなぶ。
【参考資料3】【英版R4.1.17】Nippon AMR One Health Report (NAOR) 2020 (75 ページ)
出典
| 公開元URL | https://www.mhlw.go.jp/stf/newpage_23261.html |
| 出典情報 | 国際的に脅威となる感染症対策関係閣僚会議 薬剤耐性ワンヘルス動向調査検討会(第9回 1/17)《厚生労働省》 |
ページ画像
ダウンロードした画像を利用する際は「出典情報」を明記してください。
低解像度画像をダウンロード
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
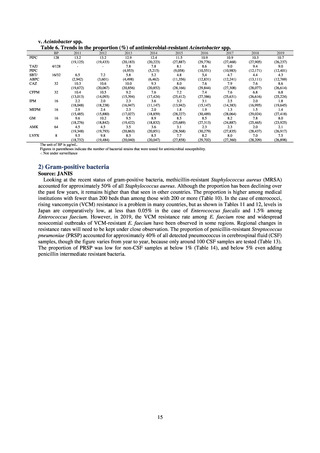
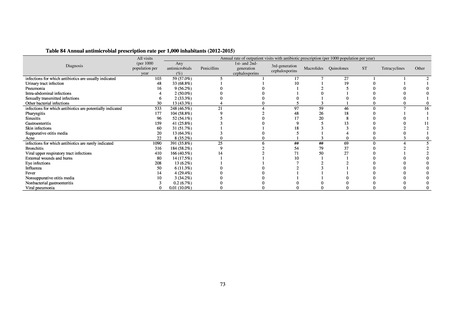
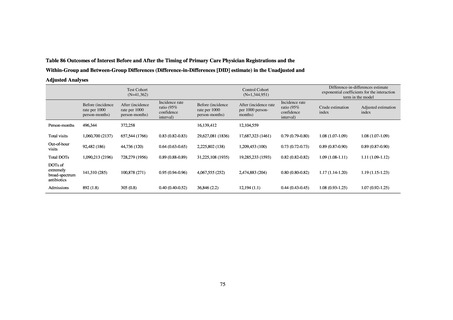
Muraki et al. used IQVIA’s database to examine the effects of the antimicrobial stewardship fee
introduced in 2018 for outpatient consultations involving pediatric patients, focusing on children under the
age of 15.5 In this study, patients were grouped according to whether or not the facility claimed the fee and
changes in the percentage of antimicrobial prescriptions for acute upper respiratory tract infections were
observed, looking at 31,137 children seen between April and August 2017 (before the fee’s introduction)
and 30,502 children seen between April and August 2018 (after its introduction). The study found that
although there fewer antimicrobials were prescribed at both facilities that claimed the fee and those that did
not after the fee was instituted (a decrease of 6.03 [4.74-7.32] percentage points and 4.84 [3.95-5.73]
percentage points, respectively), the percentage of antimicrobial prescriptions at facilities that claimed the
fee was lower (23.8% vs 34.7%, respectively, after the fee was instituted) (Table 85). Okubo et al. used the
NDB to investigate the relationship between the pediatric primary care physician registration system
introduced in April 2016 and the use of antimicrobials. 6 This retrospective cohort study tracked 1,386,313
pediatric patients aged under 2 as of April 2015 through to December 2016. A total of 41,363 patients were
registered with a pediatric primary care physician. Difference-in-differences analysis of interventions in the
group registered with a pediatric primary care physician and the group that was not found that the number
of consultations, the number of days for which antimicrobials were prescribed, and the number of days for
which broad-spectrum antimicrobials were prescribed increased (differences 1.11 [1.09-1.12] and 1.19
[1.15-1.23], respectively) among the group registered with a pediatric primary care physician, whereas a
decline in out-of-hours consultations (difference 0.89 [0.87-0.90]) was observed in that group (Table 86).
Table 85 The frequency of antibiotic prescription for URIs decreased significantly after the AS fee
implementation, regardless of whether the facility claimed the fee
Medical institutions that claimed
antimicrobial stewardship fee
Medical institutions that did not claimed
antimicrobial stewardship fee
Before introduction
After introduction
2996 (29.8%)
6345 (70.2%)
2162 (23.8%)
6925 (76.2%)
9083 (39.6%)
13880 (60.4%)
7712 (34.7%)
14505 (65.3%)
p-value*
<0.001
<0.001
*Pearson’s chi-squared test was used to verify significance
74
introduced in 2018 for outpatient consultations involving pediatric patients, focusing on children under the
age of 15.5 In this study, patients were grouped according to whether or not the facility claimed the fee and
changes in the percentage of antimicrobial prescriptions for acute upper respiratory tract infections were
observed, looking at 31,137 children seen between April and August 2017 (before the fee’s introduction)
and 30,502 children seen between April and August 2018 (after its introduction). The study found that
although there fewer antimicrobials were prescribed at both facilities that claimed the fee and those that did
not after the fee was instituted (a decrease of 6.03 [4.74-7.32] percentage points and 4.84 [3.95-5.73]
percentage points, respectively), the percentage of antimicrobial prescriptions at facilities that claimed the
fee was lower (23.8% vs 34.7%, respectively, after the fee was instituted) (Table 85). Okubo et al. used the
NDB to investigate the relationship between the pediatric primary care physician registration system
introduced in April 2016 and the use of antimicrobials. 6 This retrospective cohort study tracked 1,386,313
pediatric patients aged under 2 as of April 2015 through to December 2016. A total of 41,363 patients were
registered with a pediatric primary care physician. Difference-in-differences analysis of interventions in the
group registered with a pediatric primary care physician and the group that was not found that the number
of consultations, the number of days for which antimicrobials were prescribed, and the number of days for
which broad-spectrum antimicrobials were prescribed increased (differences 1.11 [1.09-1.12] and 1.19
[1.15-1.23], respectively) among the group registered with a pediatric primary care physician, whereas a
decline in out-of-hours consultations (difference 0.89 [0.87-0.90]) was observed in that group (Table 86).
Table 85 The frequency of antibiotic prescription for URIs decreased significantly after the AS fee
implementation, regardless of whether the facility claimed the fee
Medical institutions that claimed
antimicrobial stewardship fee
Medical institutions that did not claimed
antimicrobial stewardship fee
Before introduction
After introduction
2996 (29.8%)
6345 (70.2%)
2162 (23.8%)
6925 (76.2%)
9083 (39.6%)
13880 (60.4%)
7712 (34.7%)
14505 (65.3%)
p-value*
<0.001
<0.001
*Pearson’s chi-squared test was used to verify significance
74