よむ、つかう、まなぶ。
参考資料6_THE ESSENTIALS: CORE COMPETENCIES FOR PROFESSIONAL NURSING EDUCATION (2021 American Association of Colleges of Nursing) (18 ページ)
出典
| 公開元URL | https://www.mext.go.jp/b_menu/shingi/chousa/koutou/125/mext_00004.html |
| 出典情報 | 看護学教育モデル・コア・カリキュラムの改訂に関する連絡調整委員会(第1回 7/19)《文部科学省》 |
ページ画像
ダウンロードした画像を利用する際は「出典情報」を明記してください。
低解像度画像をダウンロード
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
© 2021 American Association of Colleges of Nursing. All rights reserved.
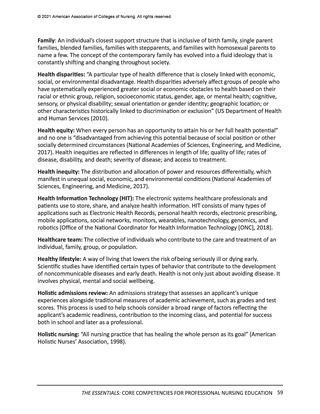
Diversity references a broad range of individual, population, and social characteristics,
including but not limited to age; sex; race; ethnicity; sexual orientation; gender identity;
family structures; geographic locations; national origin; immigrants and refugees;
language; any impairment that substantially limits a major life activity; religious beliefs;
and socioeconomic status. Inclusion represents environmental and organizational
cultures in which faculty, students, staff, and administrators with diverse characteristics
thrive. Inclusive environments require intentionality and embrace differences, not
merely tolerate them (AACN, 2017; Bloomberg, 2019). Everyone works to ensure the
perspectives and experiences of others are invited, welcomed, acknowledged, and
respected in inclusive environments. Equity is the ability to recognize the differences in
the resources or knowledge needed to allow individuals to fully participate in society,
including access to higher education, with the goal of overcoming obstacles to ensure
fairness (Kranich, 2001). To have equitable systems, all people should be treated fairly,
unhampered by artificial barriers, stereotypes, or prejudices (Cooper, 2016). Two
related concepts that fit within DEI include structural racism and social justice. (See the
glossary for definitions of structural racism and social justice.)
•
Ethics
Core to professional nursing practice, ethics refers to principles that guide a
person’s behavior. Ethics is closely tied to moral philosophy involving the study of or
examination of morality through a variety of different approaches (Tubbs, 2009). There
are commonly accepted principles in bioethics that include autonomy, beneficence,
non-maleficence, and justice (ANA 2015; ACNM, 2015; AANA, 2018; ICN, 2012). The
study of ethics as it relates to nursing practice has led to the exploration of other
relevant concepts, including moral distress, moral hazard, moral community, and moral
or critical resilience.
•
Evidence-Based Practice
The delivery of optimal health care requires the integration of current evidence and
clinical expertise with individual and family preferences. Evidence-based practice is a
problem-solving approach to the delivery of health care that integrates best evidence
from studies and patient care data with clinician expertise and patient preferences
and values (Melnyk, Fineout-Overhold, Stillwell, & Williamson, 2010). In addition
there is a need to consider those scientific studies that ask: whose perspectives are
solicited, who creates the evidence, how is that evidence created, what questions
remain unanswered, and what harm may be created? Answers to these questions
are paramount to incorporating meaningful, culturally safe, evidence-based practice
(Nursing Mutual Aid, 2020).
•
Health Policy
Health policy involves goal directed decision-making about health that is the result
of an authorized public decision-making process (Keller & Ridenour, 2021). Nurses
play critical roles in advocating for policy that impacts patients and the profession,
especially when speaking with a united voice on issues that affect nursing practice and
health outcomes. Nurses can have a profound influence on health policy by becoming
engaged in the policy process on many levels, which includes interpreting, evaluating,
and leading policy change.
THE ESSENTIALS: CORE COMPETENCIES FOR PROFESSIONAL NURSING EDUCATION 13
Diversity references a broad range of individual, population, and social characteristics,
including but not limited to age; sex; race; ethnicity; sexual orientation; gender identity;
family structures; geographic locations; national origin; immigrants and refugees;
language; any impairment that substantially limits a major life activity; religious beliefs;
and socioeconomic status. Inclusion represents environmental and organizational
cultures in which faculty, students, staff, and administrators with diverse characteristics
thrive. Inclusive environments require intentionality and embrace differences, not
merely tolerate them (AACN, 2017; Bloomberg, 2019). Everyone works to ensure the
perspectives and experiences of others are invited, welcomed, acknowledged, and
respected in inclusive environments. Equity is the ability to recognize the differences in
the resources or knowledge needed to allow individuals to fully participate in society,
including access to higher education, with the goal of overcoming obstacles to ensure
fairness (Kranich, 2001). To have equitable systems, all people should be treated fairly,
unhampered by artificial barriers, stereotypes, or prejudices (Cooper, 2016). Two
related concepts that fit within DEI include structural racism and social justice. (See the
glossary for definitions of structural racism and social justice.)
•
Ethics
Core to professional nursing practice, ethics refers to principles that guide a
person’s behavior. Ethics is closely tied to moral philosophy involving the study of or
examination of morality through a variety of different approaches (Tubbs, 2009). There
are commonly accepted principles in bioethics that include autonomy, beneficence,
non-maleficence, and justice (ANA 2015; ACNM, 2015; AANA, 2018; ICN, 2012). The
study of ethics as it relates to nursing practice has led to the exploration of other
relevant concepts, including moral distress, moral hazard, moral community, and moral
or critical resilience.
•
Evidence-Based Practice
The delivery of optimal health care requires the integration of current evidence and
clinical expertise with individual and family preferences. Evidence-based practice is a
problem-solving approach to the delivery of health care that integrates best evidence
from studies and patient care data with clinician expertise and patient preferences
and values (Melnyk, Fineout-Overhold, Stillwell, & Williamson, 2010). In addition
there is a need to consider those scientific studies that ask: whose perspectives are
solicited, who creates the evidence, how is that evidence created, what questions
remain unanswered, and what harm may be created? Answers to these questions
are paramount to incorporating meaningful, culturally safe, evidence-based practice
(Nursing Mutual Aid, 2020).
•
Health Policy
Health policy involves goal directed decision-making about health that is the result
of an authorized public decision-making process (Keller & Ridenour, 2021). Nurses
play critical roles in advocating for policy that impacts patients and the profession,
especially when speaking with a united voice on issues that affect nursing practice and
health outcomes. Nurses can have a profound influence on health policy by becoming
engaged in the policy process on many levels, which includes interpreting, evaluating,
and leading policy change.
THE ESSENTIALS: CORE COMPETENCIES FOR PROFESSIONAL NURSING EDUCATION 13