よむ、つかう、まなぶ。
資料1-2 カルベジロール 調査結果報告書及び添付文書[1.9MB] (20 ページ)
出典
| 公開元URL | https://www.mhlw.go.jp/stf/newpage_38855.html |
| 出典情報 | 薬事・食品衛生審議会 薬事分科会医薬品等安全対策部会安全対策調査会(令和5年度第15回 3/26)《厚生労働省》 |
ページ画像
ダウンロードした画像を利用する際は「出典情報」を明記してください。
低解像度画像をダウンロード
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
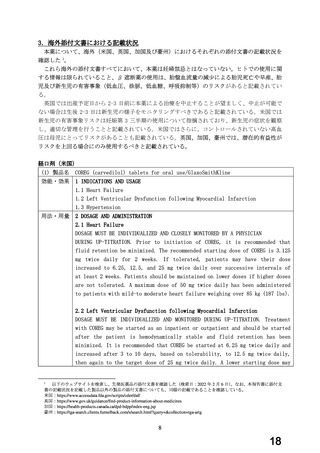
be used (3.125 mg twice daily) and/or the rate of up-titration may be slowed
if clinically indicated (e.g., due to low blood pressure or heart rate, or
fluid retention). Patients should be maintained on lower doses if higher doses
are not tolerated. The recommended dosing regimen need not be altered in
patients who received treatment with an IV or oral β-blocker during the acute
phase of the myocardial infarction.
2.3 Hypertension
DOSAGE MUST BE INDIVIDUALIZED. The recommended starting dose of COREG is 6.25
mg twice daily. If this dose is tolerated, using standing systolic pressure
measured about 1 hour after dosing as a guide, the dose should be maintained
for 7 to 14 days, and then increased to 12.5 mg twice daily if needed, based
on trough blood pressure, again using standing systolic pressure 1 hour after
dosing as a guide for tolerance. This dose should also be maintained for 7 to
14 days and can then be adjusted upward to 25 mg twice daily if tolerated and
needed. The full antihypertensive effect of COREG is seen within 7 to 14 days.
Total daily dose should not exceed 50 mg.
妊婦への
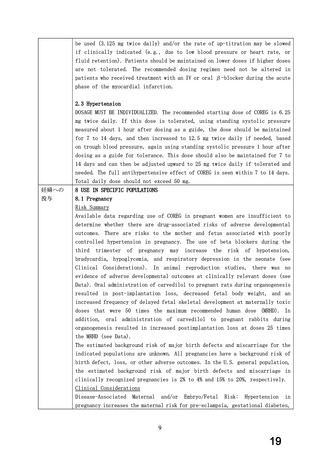
8 USE IN SPECIFIC POPULATIONS
投与
8.1 Pregnancy
Risk Summary
Available data regarding use of COREG in pregnant women are insufficient to
determine whether there are drug-associated risks of adverse developmental
outcomes. There are risks to the mother and fetus associated with poorly
controlled hypertension in pregnancy. The use of beta blockers during the
third
trimester
of
pregnancy
may
increase
the
risk
of
hypotension,
bradycardia, hypoglycemia, and respiratory depression in the neonate (see
Clinical Considerations). In animal reproduction studies, there was no
evidence of adverse developmental outcomes at clinically relevant doses (see
Data). Oral administration of carvedilol to pregnant rats during organogenesis
resulted in post-implantation loss, decreased fetal body weight, and an
increased frequency of delayed fetal skeletal development at maternally toxic
doses that were 50 times the maximum recommended human dose (MRHD). In
addition, oral administration of carvedilol to pregnant rabbits during
organogenesis resulted in increased postimplantation loss at doses 25 times
the MRHD (see Data).
The estimated background risk of major birth defects and miscarriage for the
indicated populations are unknown. All pregnancies have a background risk of
birth defect, loss, or other adverse outcomes. In the U.S. general population,
the estimated background risk of major birth defects and miscarriage in
clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated
Maternal
and/or
Embryo/Fetal
Risk:
Hypertension
in
pregnancy increases the maternal risk for pre-eclampsia, gestational diabetes,
9
19
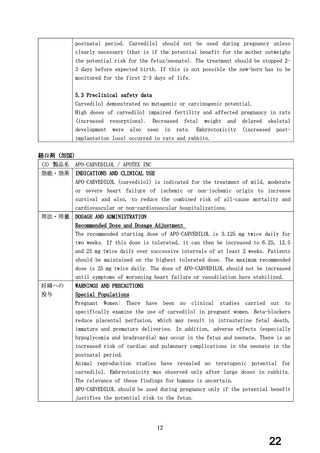
if clinically indicated (e.g., due to low blood pressure or heart rate, or
fluid retention). Patients should be maintained on lower doses if higher doses
are not tolerated. The recommended dosing regimen need not be altered in
patients who received treatment with an IV or oral β-blocker during the acute
phase of the myocardial infarction.
2.3 Hypertension
DOSAGE MUST BE INDIVIDUALIZED. The recommended starting dose of COREG is 6.25
mg twice daily. If this dose is tolerated, using standing systolic pressure
measured about 1 hour after dosing as a guide, the dose should be maintained
for 7 to 14 days, and then increased to 12.5 mg twice daily if needed, based
on trough blood pressure, again using standing systolic pressure 1 hour after
dosing as a guide for tolerance. This dose should also be maintained for 7 to
14 days and can then be adjusted upward to 25 mg twice daily if tolerated and
needed. The full antihypertensive effect of COREG is seen within 7 to 14 days.
Total daily dose should not exceed 50 mg.
妊婦への
8 USE IN SPECIFIC POPULATIONS
投与
8.1 Pregnancy
Risk Summary
Available data regarding use of COREG in pregnant women are insufficient to
determine whether there are drug-associated risks of adverse developmental
outcomes. There are risks to the mother and fetus associated with poorly
controlled hypertension in pregnancy. The use of beta blockers during the
third
trimester
of
pregnancy
may
increase
the
risk
of
hypotension,
bradycardia, hypoglycemia, and respiratory depression in the neonate (see
Clinical Considerations). In animal reproduction studies, there was no
evidence of adverse developmental outcomes at clinically relevant doses (see
Data). Oral administration of carvedilol to pregnant rats during organogenesis
resulted in post-implantation loss, decreased fetal body weight, and an
increased frequency of delayed fetal skeletal development at maternally toxic
doses that were 50 times the maximum recommended human dose (MRHD). In
addition, oral administration of carvedilol to pregnant rabbits during
organogenesis resulted in increased postimplantation loss at doses 25 times
the MRHD (see Data).
The estimated background risk of major birth defects and miscarriage for the
indicated populations are unknown. All pregnancies have a background risk of
birth defect, loss, or other adverse outcomes. In the U.S. general population,
the estimated background risk of major birth defects and miscarriage in
clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated
Maternal
and/or
Embryo/Fetal
Risk:
Hypertension
in
pregnancy increases the maternal risk for pre-eclampsia, gestational diabetes,
9
19